Ultrasound of the Week #022
Case:
A 76 year old female presented with acute severe dyspnoea at 0300, having gone to bed feeling completely well. She was a CKD5 patient on dialysis, with her last dialysis 24 hours previously.
On Examination:
A. Patent
B. Extreme respiratory distress with accessory muscle use.
Crackles throughout both lung fields anteriorly.
SpO2 <74% on room air (97% on 15L NRBM), RR38
C. Cool to mid-forearms, dry mucous membranes. BP 266/138, HR108
D. GCS15/15 but agitated.
E. Abdo SNT, calves SNT with no oedema.
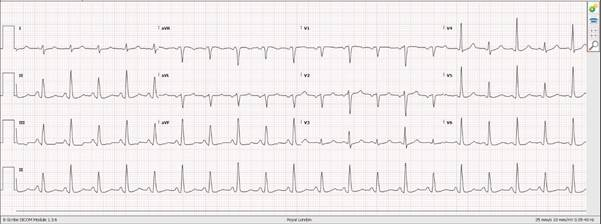
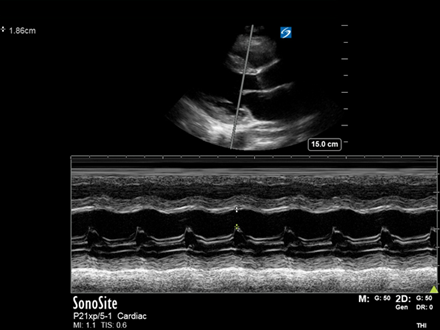
A rapid bedside lung ultrasound and echo were performed showing the following:
Question: What do you make of the lungs/echo? What does this suggest? What is the diagnosis?
[expand title=”Answer:” tag=”h2″]
The lung ultrasound shows diffuse B-lines anteriorly up to apices = interstitial syndrome (remember, ≥3 B-lines per rib space is pathological). There are no signs of pleural thickening/irregularity nor consolidation to suggest an infective process (e.g. COVID pneumonitis/pneumonia) and therefore this is highly suggestive of pulmonary oedema.
The echo is interesting in that it demonstrates an essentially normal LV systolic function and a completely flat IVC. This is not what we would usually expect in cardiogenic pulmonary oedema. Tip – B-lines with a normal LV systolic function = search for other causes of pulmonary oedema before labelling it diastolic dysfunction.
N.B. A Little Word on IVC:
Remember – the IVC is a surrogate marker for Right Atrial Pressure (RA pressure). This reflects RV preload (not necessarily LV preload) and can be raised in many conditions e.g. pulmonary hypertension, tamponade and massive PE, as well as fluid overload/congestive cardiac failure.
The utility of IVC in assessment of fluid status/responsiveness is controversial and whilst useful, an awareness of its limitations is vital.
My general rule:
- Flat IVC : RA pressure 0-5mmHg (normal) – likely fluid tolerant (not necessarily responsive)
- Intermediate IVC / varying with respiration : difficult to interpret alone.
- Plethoric IVC >21mm with little/no respiratory variation : significantly elevated RA pressures – consider above pathologies and utilise additional indicators of fluid status
Case Progression:
The findings in this case suggest:
- LV systolic failure is not the cause (although there may be diastolic failure)
- Total fluid overload is not the cause (Total body intravascular volume is likely low – it isn’t in the venous system!)
This is hypertension induced flash pulmonary oedema, otherwise known as ‘Sympathetic Crashing Acute Pulmonary Edema’ (SCAPE) – (US spelling!!).
This patient was moved to the AGP area, started on CPAP 10mmHg, 40% FiO2 (switched to BiPAP 12/8 due to pCO2 of 8.3) and GTN infusion at 100mcg/min for 2 minutes then dropped to 50mcg/min. She settled rapidly and her GTN infusion was titrated down quickly.
She was discussed with the renal SpR as she was not deemed an ICU candidate given her comorbidities. After 2 hours in the department she comfortably came off NIV and was admitted to the renal ward.
‘Sympathetic Crashing Acute Pulmonary Edema’ – SCAPE (American Spelling):
SCAPE refers to pulmonary oedema secondary to massive sympathetic drive, with fluid redistribution to the pulmonary vasculature[1]. Cardiac function can appear normal despite the massively elevated afterload[2]. These patients are not necessarily total fluid deplete, but intravascular fluid is maldistributed into the pulmonary vasculature and the lung interstitium[3]. Treatment involves respiratory support and fluid redistribution through the use of CPAP/BiPAP and IV nitrates[1,2,3].
There is a great podcast on SCAPE at EMCrit.org (see reference [3]).
References:
- Agrawal N, Kumar A, Aggarwal P, Jamshed N. Sympathetic crashing acute pulmonary edema. Indian J Crit Care Med. 2016 Dec;20(12):719-723. doi: 10.4103/0972-5229.195710. PMID: 28149030; PMCID: PMC5225773.
- Ford LE. Acute hypertensive pulmonary edema: a new paradigm. Can J Physiol Pharmacol. 2010 Jan;88(1):9-13. doi: 10.1139/Y09-113. PMID: 20130733.
- Scott Weingart, MD FCCM. EMCrit Podcast 1 – Sympathetic Crashing Acute Pulmonary Edema (SCAPE).EMCrit Blog. Published on April 25, 2009. Accessed on February 19th 2021. Available at [https://emcrit.org/emcrit/scape/].