Ultrasound of the Week #014
Case:
A 41 year old female presented reporting dyspnoea on exertion for around 18 months, with a significant deterioration in the last 4 weeks in which she had developed worsening dyspnoea on exertion and a dry cough. She had been investigated by her GP in the past for this with CXR and Echo 18 months prior to attendance and these had been reported as normal. She had no weight loss/fever/chest pain/anosmia/GI symptoms. She had no other PMH, no known COVID/ill contacts and no history of travel.
She had a bedside echocardiogram and lung ultrasound during her initial assessment, before chest XR or other investigations. This was achieved rapidly and set in motion her further investigations (CT chest).
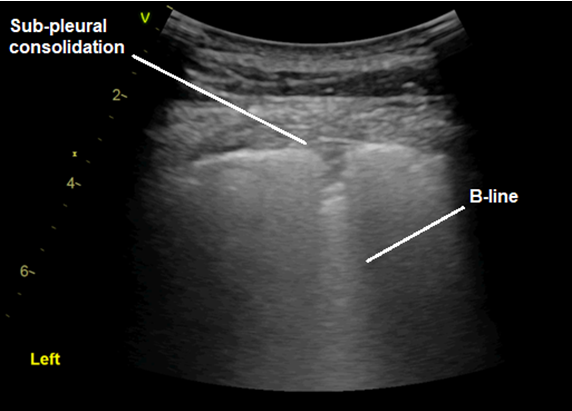
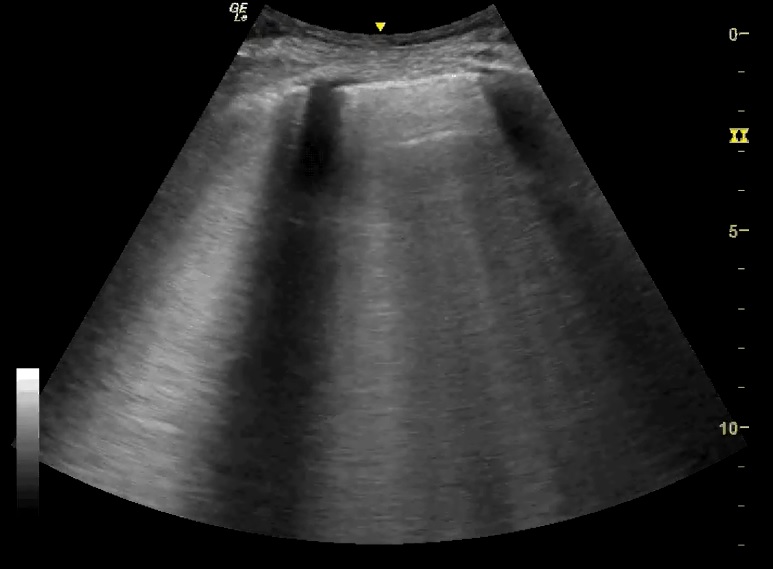
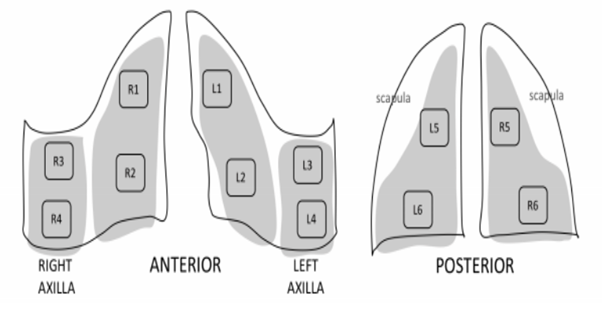
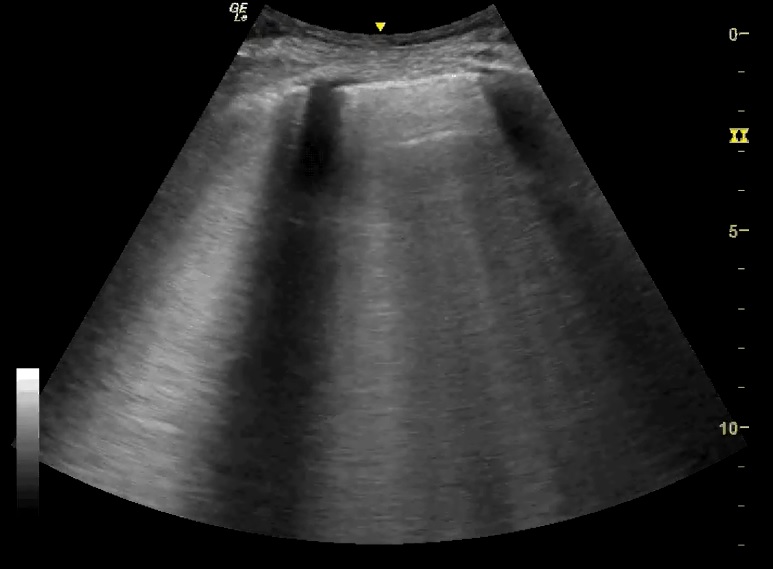
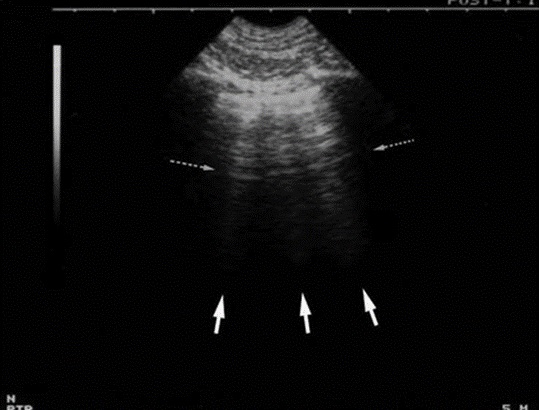
See the lung ultrasound images and key below:
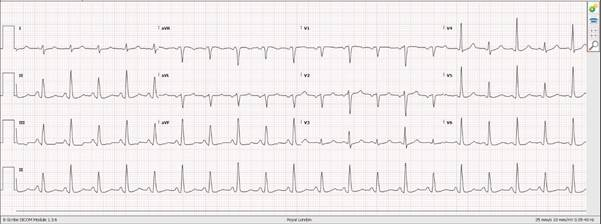
[expand title=”Echo:” tag=”h2″]
What do these images show and what could the likely diagnoses be?
[/expand][expand title=”Interpretation:” tag=”h2″]
There are diffuse B-lines throughout almost all lung fields. There were no added findings suggestive of consolidation/COVID-19 (more detail in later weeks). Bedside echo shows visually normal LVEF and no obvious abnormalities to explain her symptoms nor the lung US findings. There is always the possibility of diastolic cardiac failure, but there is no obvious LA dilation suggesting this.
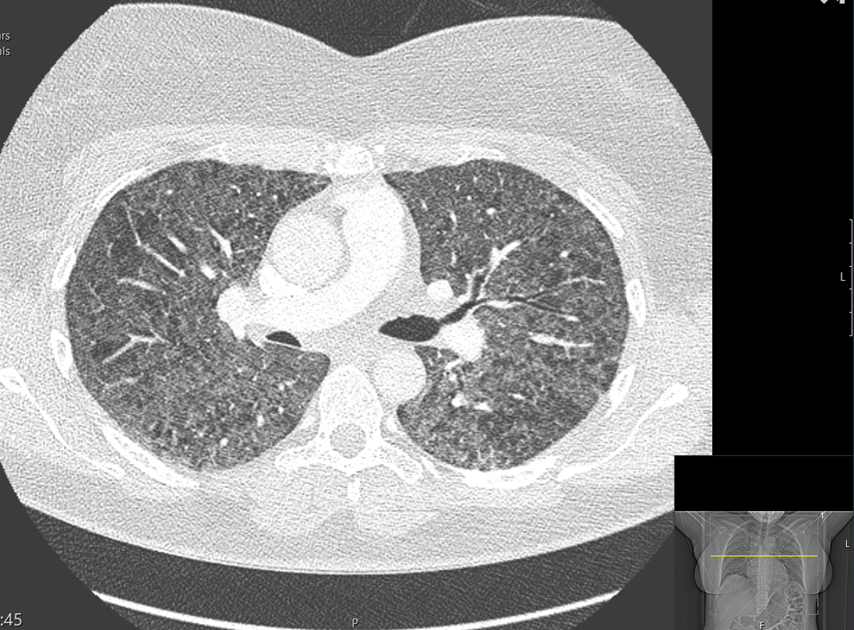
Her CTPA (shown below) was initially reported as ‘widespread centrilobular emphysema’. Given the diffuse B-lines (not found in emphysema), this was rediscussed with the on-call radiologist who agreed that there was also diffuse ground-glass changes and mosaicism with no evidence of emphysema. She is currently being investigated for Hypersensitivity Pneumonitis.
CTPA:
[expand title=”Lung Ultrasound (RCEM Level 2 Modality):” tag=”h2″]
Last week we discussed using lung US for pleural effusions, showing it is preferable to CT in terms of assessing the nature of an effusion. Remember – under normal conditions lung is aerated and therefore does not well conduct ultrasound. We can use this to our advantage in identifying pleural/pulmonary pathology through identifying changes in ultrasound artefacts, of which an important one is ‘B-line artefact’.
B-lines:
‘B-lines’ are well-defined, hyperechoic ‘comet-tail’ artefacts that arise from the pleural line and extend indefinitely. They erase A-lines (more on this in future) and move with pleural sliding[1]. They are caused by reverberation artefact and reflect sub-pleural thickened interlobular septa, present in alveolar-interstitial syndromes[1,2].
This can reflect pulmonary oedema (cardiogenic/non-cardiogenic), or other causes of interstitial inflammation or thickening (e.g. pneumonia, interstitial lung disease). There are a number of validated protocols distinguishing pathologies based on the distribution of B-lines and other artefacts.
In general, if there is a symmetrical, dependent distribution of B-lines, this greatly increases the probability of pulmonary oedema and should prompt an echocardiogram to assess for cardiac dysfunction. Indeed, distinguishing exacerbations of COPD vs. LVF is one of the most studied and powerful uses of lung US[3], and notably more sensitive & specific for pulmonary oedema compared to clinical examination, chest XR and biomarkers (BNP)[4]. Additionally, ultrasound is portable and can be used in the prehospital setting[3].
Z-lines:
‘Z-lines’ are also comet-tail artefacts arising from the pleural line but are ill-defined, short (vanish in 2-4cm), don’t move with lung sliding and don’t erase A-lines. They have no pathological significance and should not be confused with B-lines.
In this case, lung ultrasound both expedited investigations and admission, and facilitated questioning of CT findings with radiology/respiratory colleagues.
[/expand]References:
- Lee FC. Lung ultrasound-a primary survey of the acutely dyspneic patient. J Intensive Care. 2016 Aug 31;4(1):57. doi: 10.1186/s40560-016-0180-1. PMID: 27588206; PMCID: PMC5007698.
- Dietrich CF, Mathis G, Blaivas M, et al. Lung B-line artefacts and their use. J Thorac Dis. 2016;8(6):1356-1365. doi:10.21037/jtd.2016.04.55
- Zanatta M, Benato P, De Battisti S, Pirozzi C, Ippolito R, Cianci V. Pre-hospital lung ultrasound for cardiac heart failure and COPD: is it worthwhile?.Crit Ultrasound J. 2018;10(1):22. Published 2018 Sep 10. doi:10.1186/s13089-018-0104-5
- Pivetta E, Goffi A, Nazerian P, Castagno D, Tozzetti C, Tizzani P, Tizzani M, Porrino G, Ferreri E, Busso V, Morello F, Paglieri C, Masoero M, Cassine E, Bovaro F, Grifoni S, Maule MM, Lupia E. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: a randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-766. doi: 10.1002/ejhf.1379. Epub 2019 Jan 28. PMID: 30690825.