Ultrasound of the Week #016
Case:
A 64 year old male with a PMH of asthma, hypertension and Type 2 Diabetes presented with gradual onset central chest tightness worse on exertion, associated shortness of breath and feeling hot for 8 days. He had no other symptoms of note.
Examination revealed scattered bibasal crackles on auscultation but no other abnormalities.
SpO2 93% RA, 80% on exertion. HR96, T37.5, RR20, BP 136/78.
He had a lung ultrasound and bedside echo:
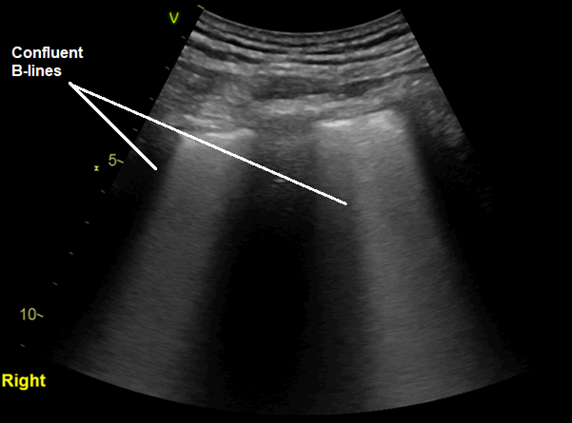
Lung US:
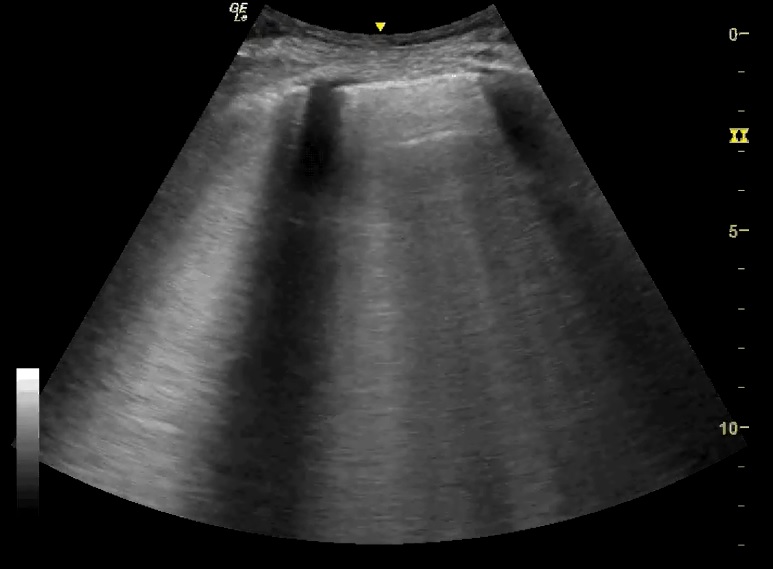
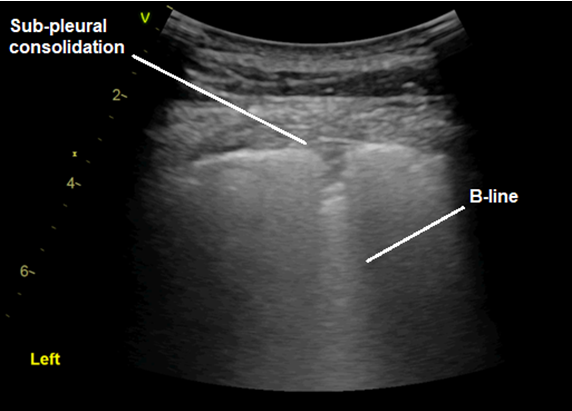
Left lung
Right lung
[expand title=”Echo:” tag=”h2″]
The echo is essentially normal, with no signs of right heart strain nor LV dysfunction. The focus here is on the lung ultrasound.
There are diffuse B-lines that in many places are coalescing, pleural irregularity and areas of sub-pleural consolidation. Remember, B-lines represent ‘alveolar-interstitial syndromes’ (pulmonary oedema, inflammation). We see these most commonly in pulmonary oedema. However, given a normal bedside Echo and especially the pleural thickening and sub-pleural consolidation, this is highly suggestive of a diffuse inflammatory process which in this case is most likely COVID-19 pneumonia.
This patient was admitted under the medical team. As he had a normal lymphocyte count, low CRP, was tachycardic and had pleuritic chest pain he had a CTPA which was reported as:
“No pulmonary embolism identified. Bilateral new peripheral ground-glass opacification is highly suspicious of COVID-19 pneumonia. Correlation with RT-PCR is recommended”
[expand title=”Lung Ultrasound in COVID-19:” tag=”h2″]
Lung ultrasound has been put to great use in the COVID-19 pandemic in many countries, from streaming patients to tracking progression of disease in ICU and titrating therapy according to findings[1], and more evidence continues to be published on it’s utility. The sensitivity of Lung Ultrasound for signs of viral pneumonia is considerably higher than chest XR[2] and approaches that of CT.
The classic findings in viral pneumonia are[3]:
- B-lines, focal and confluent
- Irregular or thickened pleural line
- Sub-pleural consolidation
- Small or no pleural effusions (large effusions are uncommon in COVID-19)
- Dense consolidation with air bronchograms in more severe disease
Lung ultrasound can identify features strongly supporting a diagnosis, map progression of disease and most importantly assess for alternative diagnoses[4] (e.g. pneumothorax, pleural effusions).
[/expand]References:
- Moore S, Gardiner E. Point of care and intensive care lung ultrasound: A reference guide for practitioners during COVID-19. Radiography (Lond). 2020 Nov;26(4):e297-e302. doi: 10.1016/j.radi.2020.04.005. Epub 2020 Apr 17. PMID: 32327383; PMCID: PMC7164867.
- Shumilov E, Hosseini ASA, Petzold G, Treiber H, Lotz J, Ellenrieder V, Kunsch S, Neesse Comparison of Chest Ultrasound and Standard X-Ray Imaging in COVID-19 Patients. Ultrasound Int Open. 2020 Sep;6(2):E36-E40. doi: 10.1055/a-1217-1603. Epub 2020 Sep 2. PMID: 32905446; PMCID: PMC7467801.
- Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020